Abstract
In patients with acute myeloid leukemia (AML), more common aneuploid alterations, such as complex- or monosomal karyotype (CK and MK, respectively) have been intensively studied and are known to confer an adverse prognosis. In contrast, little is known about the prognosis of clonal tetraploidy/near-tetraploidy (T/NT), another rare aneuploidy, defined by presence of 92 chromosomes in tetraploid, and 81-103 chromosomes in near-tetraploid cases. Therefore, we aimed to evaluate prevalence, clinical as well as molecular characteristics and prognostic impact of T/NT in a large cohort of AML patients.
We retrospectively assessed 4259 AML patients treated within Study Alliance Leukemia (SAL) trials and/or registered in the SAL AML registry and for whom valid cytogenetic data were available from 1996 until 2020 (the cohort was subsequently enriched by 5 T/NT cases from the AML cooperative group (AMLCG) AML registry). T/NT was defined by presence of ≥ 81 chromosomes in ≥ 10% of metaphases in G-banded karyograms and/or ≥ 4% T/NT cells in interphase fluorescence in-situ hybridization (iFISH). Bone marrow mononuclear cell (BMMC) nuclear area was assessed in patients with available bone marrow smears. In 22 patients with available BMMCs were available, panel next generation sequencing (NGS) and/or whole genome sequencing (WGS) was performed. Student's t test and Kaplan-Meier estimation were used for statistical analyses.
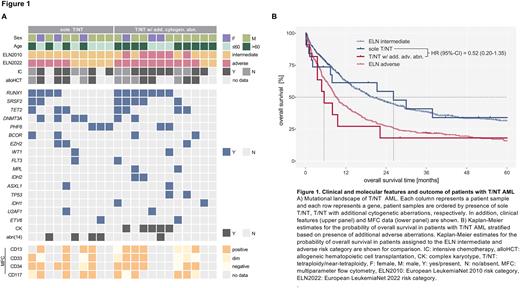
We identified 35 patients with T/NT (prevalence 0.82%). Median age was 60.1 years, 34.2% were female. Most patients were diagnosed with de-novo AML (77.2%); secondary AML and therapy-related AML was seen in 20.0% and 2.8%, respectively. Median WBC was 2.9 ×109/L, platelet count was 59 ×109/L and hemoglobin was 6.2 mmol/L; median bone marrow blast count was 64%. As per standard of care molecular studies, there was no evidence of biallelic CEBPA or NPM1 mutations, only one patient harbored an FLT3-ITD mutation; a complex karyotype was observed in 22.9%. In 24 patients considered fit/eligible for intensive chemotherapy (IC) the CR rate was 54.2%, allogeneic hematopoietic cell transplantation (HCT) was performed in 34.2% of patients. As compared to AML patients with diploid karyotype, median BMMC nuclear area was increased (209 µm2 vs. 129 µm2, p = .02). NGS/WGS revealed an accumulation of RUNX1 (15 variants in 11/22 patients), TET2 (15 alterations in 7/22 patients) and SRSF2 (7 variants in 7/22 patients) mutations. Moreover, frequent chromosome 14 aberrations, e.g. del(14q) were observed (5/22 patients). In contrast, only two patients harbored FLT3 mutations and no variants in CEBPA or NPM1 were seen; also, CBF fusions and KMT2A rearrangements were absent (Figure 1A). Median overall survival (OS) of the entire cohort was 9.6 months. Of note, when evaluating patients with sole T/NT vs. patients with T/NT and additional adverse aberrations, median OS in T/NT patients without additional adverse alterations was 26.1 months vs. 5.5 months in patients with T/NT and adverse risk (Figure 1B). Thus, T/NT per se do not seem to confer an adverse prognosis.
In summary, we report the first comprehensive evaluation of AML patients with T/NT. T/NT was associated with distinct clinical (male predominance, large BMMC nuclear area) and molecular features (mutations in RUNX1, TET2, SRSF2; del(14)). Most importantly, isolated T/NT was not associated with a poor prognosis; accordingly, we suggest assigning AML patients with T/NT without additional adverse-risk alterations to the intermediate-risk category.
Disclosures
Ruhnke:Beigene: Other. Jost:BMS Celgene: Honoraria; Jazz: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal